Today, we are going to explore a lab that was conducted in class this week. The goal of this lab was to monitor the electrical activity of the masseter muscle as different foods were eaten, and discover which foods require the most electrical activity. To accomplish this, a group member attached monitors to their cheek and forearm, and ate four different foods. For a constant variable, we also tracked the electrical activity of the jaw when it was at rest and when it was clenched.
As the monitor collected data, it recorded it in a chart where wavelengths were visible and could be measured. These charts can be seen below.
Penut Butter and Jelly Sandwich Chart
Cookie Chart
Ruffles Potato Chips Chart
Oreo Ball Chart
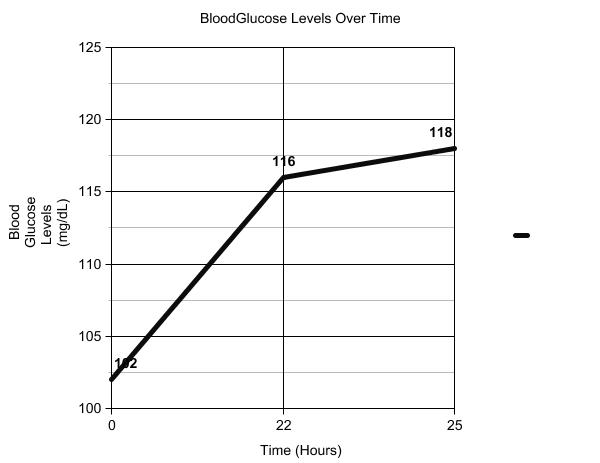
Compiled mV Data
Relaxed Jaw/Clenched Jaw Chart
To find the delta mV, we measured the Maximum mV of a given wave and subtracted the Minimum mV from it. The resulting number was then graphed. We repeated this process for the constant variables and the other foods.
The graph below illustrates the compiled data from the experiment.
The results from this lab were very different than my hypothesis- the complete opposite, in fact. I thought that the chips would require more electrical activity, as the initial bite is more difficult than the initial bite of the PB&J. I did not take into account, however, the following bites. The chip became easier to chew the longer it was in the subject's mouth, while the PB&J only varied slightly. It is also more difficult to complete the bite through a sticky substance than it is to take a quick, sharp bite from a chip, which I had not thought about, either. It would be very interesting to repeat this lab with different, more diverse foods, such as steak and raw carrots. This would show more varying results than those reflected in the original experiment.
Thanks for joining in the exploration of electrical muscle activity!